Abstract
Introduction:
The utility of bleeding assessment tools (BAT) as predictors of bleeding diatheses has been well established, but their utilization in the current era of electronic medical records is limited by their tediousness. Self-administered bleeding questionnaires are increasingly recognized as valid tools for guiding coagulation evaluation, shifting the onus from physicians to patients. A recent study by Casey et al evaluated use of a self-administered pediatric bleeding questionnaire (self PBQ), but the focus was on validation of the tool for screening of von Willebrand disease, and the results have not been replicated. Also, the self-PBQ, still being pen-paper based, has similar limitations as other BATs.
Our study evaluates the use of an electronic version of the self-administered pediatric bleeding questionnaire through a tablet/smart device - an "eBAT", with patients and their parents reporting the patient's bleeding symptoms prior to a hematology evaluation visit.
Objectives:
Primary objective was to determine the accuracy of the patient/parent self-administered eBAT by determining the level of agreement between patient/parent response and physician interview based response to the same bleeding report questionnaire (P-BAT).
Methods:
New patients referred to a pediatric hematology clinic for evaluation of a possible bleeding disorder were approached to participate in this study. Consenting families answered the bleeding questionnaires twice - once via a self-administered eBAT questionnaire on a tablet device via REDCap® and once through a physician administered version. The participants were randomly assigned to completing the eBAT first or the P-BAT first. The questionnaire utilized has been validated for use for minimum grade 4 reading level and patients older than 9 years of age were allowed to respond to the questionnaire themselves with help from their parents.
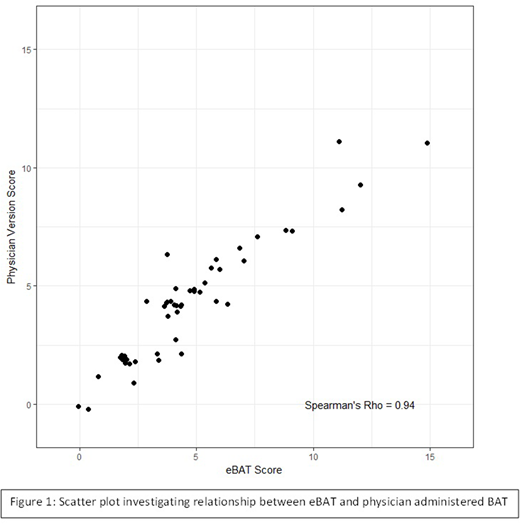
We carried out an interim analysis as designed a priori for the study results. We assessed the correlation between eBAT and P-BAT scores and calculated the Spearman's correlation coefficient and Cochran's Kappa statistic (≥ 0.6 reflecting substantial and ≥0.9 reflecting almost perfect degrees of agreement).
Results:
As part of the interim analysis, we studied 48 questionnaire response pairs. Median age of subjects was 12.8 years (range: 0.04 - 20.99). The median time required for patients or parents to complete the eBAT was 6 minutes (2 - 28), with only 25% patients (n=12) requiring longer than 10 mins. There was very strong correlation of bleeding scores noted when comparing eBAT and P-BAT scores, (Spearman's correlation coefficient 0.94, Figure 1). A weighted Kappa statistic for the comparison between self eBAT and P-BAT was 0.697; indicating substantial agreement between the bleeding scores based upon physician interviews and self-reported symptoms (p-value <0.0001). On the eBAT, 75% (n=36) of patients had scores considered abnormal for children (≥3), whereas 68.8% (n=33) of patients had abnormal scores with the P-BAT (p=0.25). Out of this population, 43.8% (n=21) of patients had a specific bleeding diathesis diagnosis (von Willebrand disease or low von Willebrand factor levels, n=8, platelet function abnormality or platelet storage pool disease, n=6, other factor deficiencies, n=5 or transient coagulation abnormalities due to inhibitors, n=2). The eBAT scored per the self-PBQ based key had a sensitivity of 77.3% (95 % CI 54.6 - 92.2%), a specificity of 28% (95 % CI 12.1 - 49.4%), a positive predictive value of 48.6% (95 % CI 40.4 - 56.9%) and a negative predictive value of 58.33 % (95% CI: 34.12 - 79.10%) for identifying a bleeding disorder.
Conclusions & Future Directions:
In a pediatric hematology specialty clinic setting, the information gained from the eBAT was noted to be very comparable to the physician administered bleeding questionnaire in this interim analysis, with 75% of participants being able to complete the eBAT in under 10 minutes. The clinical application of eBAT has the potential to improve utilization of bleeding scores in the evaluation of patients with possible bleeding diatheses by addressing the limitations of a paper-pen based survey.
Future work will focus on translating the electronic information from the eBAT to the patient medical record in real time, in the form of pertinent history data and bleeding scores.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal